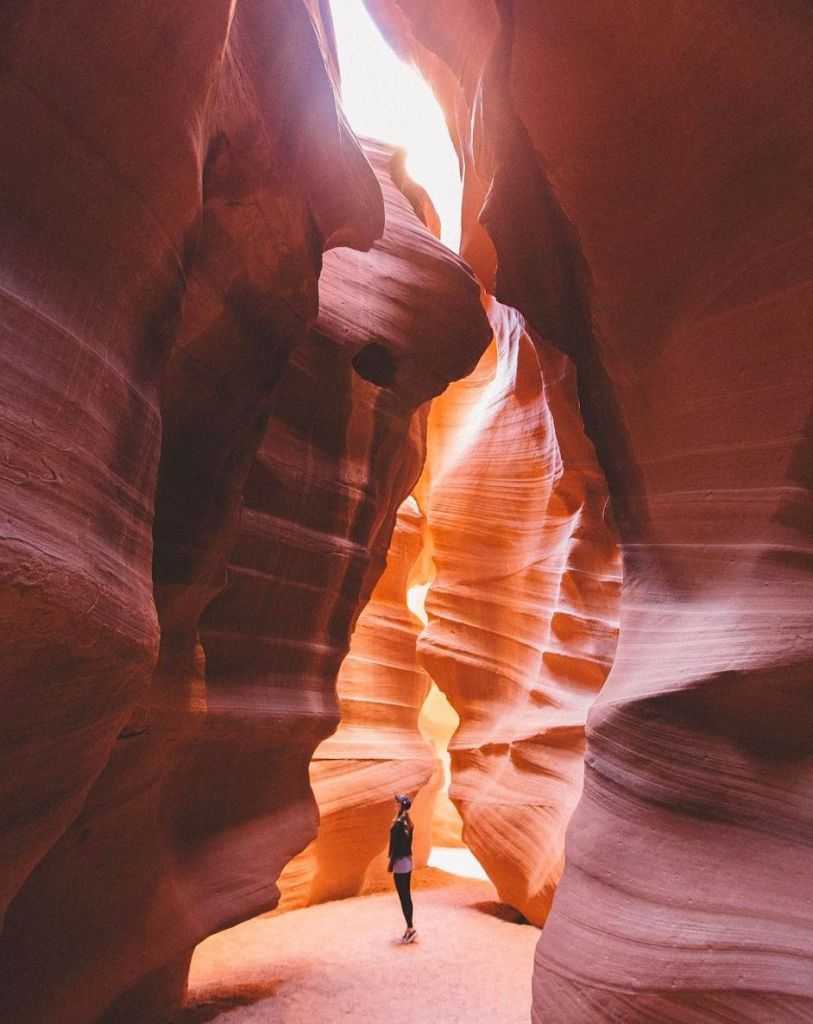
If you’re anything like us, you find yourself sucked into the Instagram rabbit hole every once in a while. And who can blame you? Not only is Instagram a fantastic way to discover new events, products and companies, but the popular social media platform also provides a way to unwind and appreciate truly spectacular photography.
The following list features some of Canada’s own local talent, allowing us to visually explore the country’s great mountains, grasslands, oceans, food, and people. Get inspired and check out these fourteen amazing Canadian photographers on Instagram. You can also discover these and other great images using #BeautifulCanada.
Based out of Edmonton, Alberta, Martina Gutfreund posts colourful, breathtaking scenes of the snow-capped Rockies and peaceful Provincial Parks in her area, all alongside her furry travel companions.
Hailing from Vancouver Island and the Edmonton area, Brie and Reuben are a Vancouver-based photography duo with an eye for adventure.
Flo Lum takes stunning photographs of Vancouver, BC and the surrounding Lower Mainland. She has a way of using interesting angles and mixing up her feed with images of nature, food, and family.
Karlynn Johnston is a food and travel writer from Edmonton who takes titillating food photographs of her cookbook creations as well as delicacies from her travels across the country and abroad.
An avid explorer of BC, Brayden Hall is an adventure photographer and professional drone pilot who captures stunning aerial photos of the province’s most beautiful landscapes.
Husband to Flo Lum (what a team!), Dan Lum takes incredible photos of the British Columbia wilderness and landscape. His way of using perspective always tells an intricate story in each photograph, from sea to sky, forest to mountains.
A resident of the Northwest Territories for almost a decade, Adam Hill’s images of the True North reveal mesmerizing waves of aurora and intricate portraits of wildlife. His work has been featured in Canadian Geographic and Outdoor Photographer Magazine, to name a few.
If you haven’t been following the photo adventures of Andrew Knapp and his adorable border collie Momo, you’ve been missing out. By incorporating his canine companion into gorgeous wilderness backdrops, he’s created a new style of travel photography.
Based in Vancouver, Emma Choo shares delectable photographs of her city’s amazing international and local cuisine. Her photos are vibrant, enticing, and guaranteed to make you drool.
JongSun Park is a Vancouver-based photographer keeping a daily photo diary of his life. From cafés, antique shops, and motorcycles, JongSun captures the city from a vintage-inspired lens that takes you back in time.
From Canmore, Alberta, Chris Sheremata’s photographs range from serene lake views to incredible glacial ascents, and from hypnotizing starry mountain skies to collaborative bouldering adventures.
Not only do Brooke Willson’s photographs feature inspiring mountain ranges and sprawling waterfront views, but the inclusion of her dog Timber appeals to all the dog lovers who never leave home without their pup.
Paul Zizka is an award-winning landscape and adventure photographer hailing from Banff, Alberta. He has has explored the peaks of his native Rockies and beyond, all while capturing the natural beauty of the surrounding ice, rock, sea, and sky.
Kari Medig is a photographer who grew up in northern BC, now living in Nelson. He shoots in film, which gives his images a dreamlike quality, and many feature snowcapped mountains. Kari has shot for several Canadian publications, including Destination BC, the Globe and Mail, and Air Canada’s enRoute.
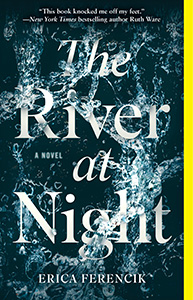 The River at Night by Erica Ferencik
The River at Night by Erica Ferencik