Summer provides many opportunities to get outside and have fun, but that fun can be spoiled by summer health hazards. Sunburns, bug bites, allergies, injuries, and infections can all play a role in how much you get to enjoy your summer. If you want more fun and less pain, it is important to take preventive measures to protect yourself and your family. Fortunately, there are steps you can take to prevent these problems and relieve the discomfort they can cause. One of the best steps is to consult your pharmacist about preventing and treating potential problems. Remember, some pharmacists can even prescribe medications to treat minor ailments such as insect bites and stings, rashes, sunburn, and muscle sprains and strains.
Summer provides many opportunities to get outside and have fun, but that fun can be spoiled by summer health hazards. Sunburns, bug bites, allergies, injuries, and infections can all play a role in how much you get to enjoy your summer. If you want more fun and less pain, it is important to take preventive measures to protect yourself and your family. Fortunately, there are steps you can take to prevent these problems and relieve the discomfort they can cause. One of the best steps is to consult your pharmacist about preventing and treating potential problems. Remember, some pharmacists can even prescribe medications to treat minor ailments such as insect bites and stings, rashes, sunburn, and muscle sprains and strains.
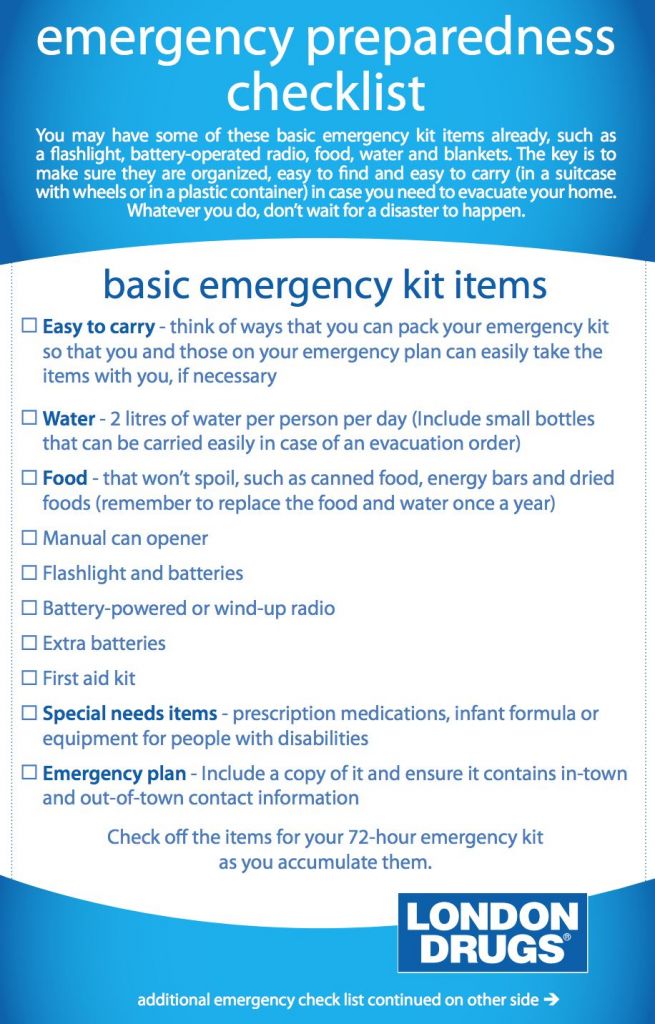
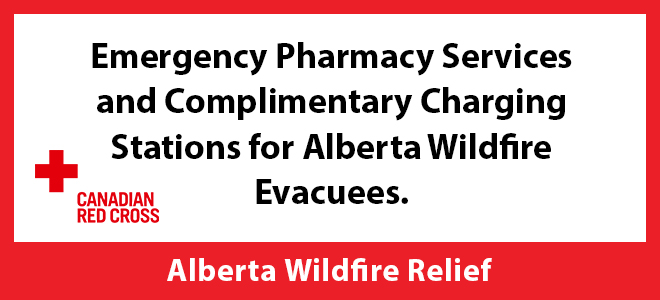
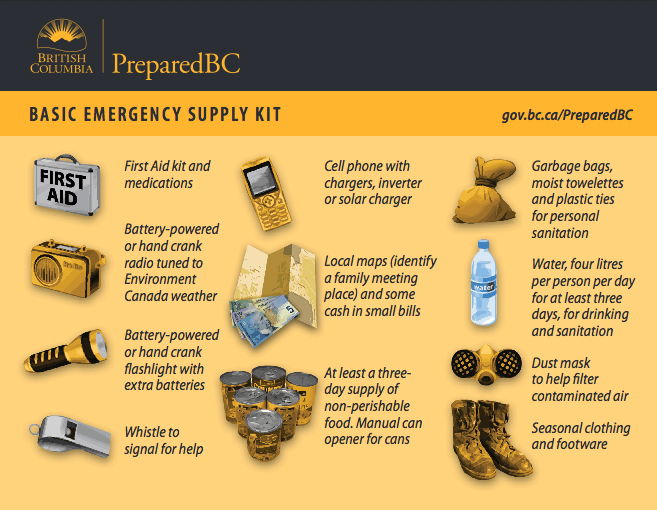
One of the ways you can prepare to deal with summer health hazards is to create a summer health kit so you will have the items you will need if a problem does occur. Your London Drugs pharmacist can help you customize your kit, but the chart below outlines some of the products that you should consider having in your kit.
| Problem | Helpful Products | Tips |
| Itching & Allergies | · Topical anti-itch creams (e.g., hydrocortisone, calamine) soothe bites and mild rashes. · Oral antihistamines (e.g., loratadine, cetirizine) reduce swelling, itching, and allergic reactions from bites, stings, or seasonal allergens. | Always ask a pharmacist before combining oral and topical antihistamines. Note: Pharmacists can prescribe treatments for allergy symptoms or persistent insect bites.
|
| Pain from Sprains & Strains | · Analgesics like acetaminophen or ibuprofen help manage pain and reduce inflammation from overexertion, minor injuries, or sun headaches. · Topical analgesics (e.g., diclofenac gel) provide targeted muscle and joint pain relief. · Hot/cold packs · Athletic wraps and supports | Pharmacists can assess and prescribe medicines for muscle sprains/strains, helping you recover faster without a clinic visit. |
| Skin Rash & Minor Infections | · Antibiotic ointment/cream · Sterile saline for wound cleansing · Sterile gauze pads and bandages · Antifungal cream
| Keep in mind that heat, sweat, and sun can cause rashes or minor skin infections. Pharmacists can assess and prescribe treatment for skin rashes, mild fungal infections, or eczema flare-ups, preventing the need for a doctor’s visit in many cases. |
| Sunburn | · Aloe vera gel offers cooling relief and supports skin healing. · Sterile saline water can be used to clean blisters or soothe inflamed skin. · Non-scented moisturizers help restore moisture and reduce peeling. | Apply SPF 30+ broad-spectrum sunscreen—pharmacist-recommended options are available. Don’t forget lips, ears, scalp, hands, and tops of feet. |
| Tick Removal & Insect Protection | · Insect repellents containing DEET or icaridin. · A tick removal kit that includes fine-tipped tweezers, antiseptic, and a sealable bag for tick storage. | Wear long sleeves when hiking and do daily tick checks. Reminder: Pharmacists can offer advice on removal and risk of Lyme disease. They may also prescribe treatment for mild tick bites or related skin reactions. |
It is also important to have a well-stocked basic first aid kit handy plus a travel-sized kit to take with you when you are away from home. Your pharmacist can advise you on what items you should include in your kit to customize it for your personal needs, but among the items to consider are those listed in the chart above plus:
- Adhesive tape
- Antiseptic wipes
- Roller bandages to hold dressings in place or to make an arm sling
- Blister pads
- Burn cream
- Disposable non-latex gloves
- Small sealable bag for tick storage
- Sterile gauze pads in several sizes
- Tweezers and scissors
Having a summer-ready first aid kit saves times, prevents complications, and supports a fun, worry-free season. Whether you’re hitting the trails, beach, or backyard, your pharmacy is a trusted resource for your health products and advice, and it should be your first stop for smart summer health.