 Physical activity is the best treatment for type 2 diabetes. Why not do it in the great outdoors?
Physical activity is the best treatment for type 2 diabetes. Why not do it in the great outdoors?
Exercise is considered one of the cornerstones of treatment for people living with type 2 diabetes for a host of reasons: it improves the body’s use of insulin, burns excess body fat, improves muscle strength and heart health, increases bone density, lowers blood pressure, relieves stress, lifts one’s mood, and increases energy.
Exercise doesn’t just make you feel better, it also reduces disease, lessens hospitalizations, and can actually help you live longer. A 2012 study of 650,000 people from the U.S.-based Brigham and Women’s Hospital and the National Cancer Institute proved just that. It found that people over 40 who walked briskly for 75 minutes per week lived an extra 1.8 years. That increased to 3.4 years when they walked 150 to 299 minutes per week and to 4.5 years for 450 minutes per week.
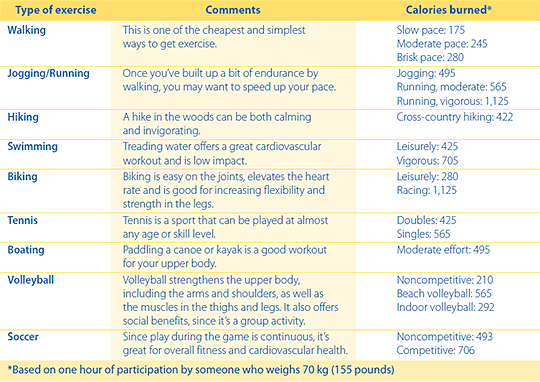
 The Canadian Diabetes Association recommends at least 30 minutes of moderate activity five days a week for a total of 150 minutes of exercise. If you hate the idea of hitting the gym for a workout, there are plenty of other fun— yes, fun!—ways to work in that exercise.
The Canadian Diabetes Association recommends at least 30 minutes of moderate activity five days a week for a total of 150 minutes of exercise. If you hate the idea of hitting the gym for a workout, there are plenty of other fun— yes, fun!—ways to work in that exercise.
Spring is a time when many people start thinking about kick-starting a new exercise program or ramping up their existing routine. With the onset of warm weather and longer days in the summer, why not consider one or more of these outdoor activities as a way to keep fit?

Before you exercise: 7 tips for getting started
- Meet with your doctor or certified diabetes educator to discuss an activity plan that’s best for you. It’s best not to participate in any exercise more vigorous than brisk walking before consulting with your doctor to ensure the exercise program is safe for you.
- Wear comfortable socks and shoes that fit well to prevent foot irritation. Be sure to check your feet for blisters or sores after exercising, since foot irritations can lead to serious infections in people with diabetes.
- Drink plenty of water—dehydration may occur during exercise and can affect blood sugar levels.
- Exercise can lower blood sugar. If you are on insulin or one of the many glucose- lowering pills, it is important to always carry glucose tablets or another sugar source such as Life Savers®. By doing so you will be prepared in case you experience low blood sugar. Your pharmacist can tell you if the medication you take puts you at an increased risk for low blood sugar.
- Bring your glucose meter with you and check your blood sugar level before, during, and after you exercise so you can take action if your blood sugar drops too low.
- If you take insulin, you may need to adjust your dose before exercising. Your doctor or certified diabetes educator can advise you on this.
- Start slow and gradually increase your endurance. If you haven’t exercised in a while, don’t overdo it!

